Introduction: A 483 Form, Unveiling the Mysteries of Sterile Production
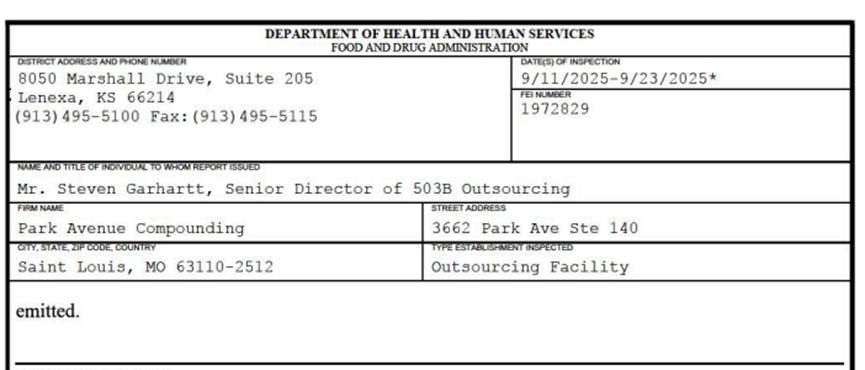
In September 2025, the U.S. Food and Drug Administration (FDA) conducted a nearly two-week inspection of Park Avenue Compounding. Following the inspection, the FDA issued a 14-page FDA Form 483 to the company, detailing eight key observation items ranging from aseptic process validation, environmental control, deviation management to data integrity, covering nearly every core pillar of Good Manufacturing Practice (cGMP). This report is not merely a regulatory document for a single company but serves as a mirror reflecting the widespread quality system deficiencies and compliance risks in the sterile preparation manufacturing industry. This article will conduct an in-depth analysis of the Form 483 report to reveal the industry-wide issues and the lack of management philosophy reflected therein.
I. The Foundation of Sterility Assurance Shaken: Process Validation and Cleaning & Disinfection
1.1 Lack of "Representativeness" in Medium Filling Validation
Observation 1 directly addresses the core of aseptic process validation—the adequacy of medium filling. The FDA found that the company's medium filling did not simulate its actual production of the "maximum batch size." This means that the critical validation for demonstrating the ability of aseptic operators, environment, and processes to sustain the production of sterile products failed to cover the worst-case production conditions. More concerning is the company's failure to provide "sufficient scientific justification" for this scale discrepancy.
Deep-seated issues: This exposes the formalism in corporate quality risk management. Medium filling should not be a compliance project conducted merely for verification's sake, but rather a practice grounded in science and risk assessment, simulating worst-case conditions, and challenging the limits of sterility assurance. When validation design is detached from actual production scenarios, the resulting "sterility assurance" conclusions become meaningless. Furthermore, records indicate that medium units were unjustifiably destroyed prior to cultivation, with no corresponding written procedures in place, demonstrating arbitrariness and uncontrollability in the validation execution process, which further undermines the reliability of validation data.
1.2 Sterile Area Cleaning: Behavioral Deviance and System Failure
Observation 2 described a shocking scene witnessed by inspectors on September 19,2025: Contractual technicians responsible for the 'terminal cleaning' of the ISO-7-grade buffer room adjusted sterile boots with gloved hands, resulting in skin exposure; while kneeling behind the ISO-7 floor cleaning equipment, they continued working without changing the contaminated sterile suits and boots.
The underlying issue: This is far from an isolated operational error, but rather a clear sign of systemic failure in the Cleanroom Sanitation System (SDSS). First, the critical task of maintaining a sterile environment—cleaning—has been outsourced to third parties who may lack adequate training or oversight. Second, the blatant violation of basic changing room and cleanroom protocols being observed highlights a severe lack of daily supervision and a quality culture on-site. A cleanroom environment isn't built with hardware, but with every standardized action taken by every person entering it. When standards are breached, even the best-designed hardware becomes meaningless.
II. The Double Failure of Environmental Control and Risk Management
2.1 Airflow: The Ineffective 'Invisible Guardian' of Sterile Operations
Observation 3 indicates that the June 2025 smoke test demonstrated that the unidirectional airflow in the ISO-5 Class core operating area had been disrupted under dynamic conditions, resulting in vortex and turbulence. A specific scenario occurred when an operator leaned against the workbench, causing turbulence to impact their chest and backflow, potentially contaminating the ISO-5 Class clean air. Unidirectional airflow serves as the lifeline ensuring that aseptic operating areas remain free from particulate and microbial contamination, and its failure directly threatens the sterility of the product.
Root cause analysis: This finding indicates potential deficiencies in facility design qualification (DQ), operation qualification (OQ), and performance qualification (PQ), or that routine monitoring and maintenance failed to detect performance drift. More critically, the company lacked an effective response to this high-risk scenario. The personnel monitoring protocol was poorly designed (using rotating sampling points instead of full coverage) and lacked risk assessment to justify its statistical methodology, resulting in monitoring data that failed to accurately reflect the actual environmental impact of production activities.
2.2 Risk Assessment: Theoretical Discussion and Realistic Application
The deficiencies in the VAL-24-001 risk assessment document are highly representative: it failed to evaluate the airflow impact of material transfer from low-level areas to ISO-7 areas; did not provide scientific justification for environmental monitoring frequency; and neglected to monitor pressure differentials to ensure airflow direction. Critically, this risk assessment was completed prior to the company's implementation of "standard aseptic operations," yet identified the material transfer pathway as "highest risk." A risk assessment that should have been based on actual operational data and potential failure modes, completed in advance and not updated with operational realities, is akin to working in isolation, failing to identify and control genuine risks.
The underlying issue exposes a common pitfall in current enterprise risk management practices: treating risk assessment as a static, one-time "compliance document" rather than a dynamic, knowledge-based, and continuously iterative management process. Evaluations detached from practical operations fail to provide actionable insights for decision-making, leading to misallocation of resources and overlooking genuinely high-risk areas.
III. The Vicious Cycle of Deviation Handling and Quality Control
3.1 CAPA's' Idle 'and the' Cycle' of Deviation
Observations 4 and 6 outline a picture of a paralyzed deviation management system. Case 1: A batch of norepinephrine contained an API dose error due to the use of an incorrect specification syringe, resulting in a potency of 0%. The corresponding CAPA-25-005 erroneously referenced the master batch record for "oxytocin," and the corrective actions were not implemented in the relevant master batch records. Case 2: A potassium chloride batch had a potency of 0% due to calibration deviations in the filling pump, with a risk level of "high," yet it was approved for release by personnel authorized as QA managers. The corresponding CAPA-25-006 again incorrectly referenced records for another product.
The core mission of the CAPA system is to "correct" and "prevent" recurrence. When the CAPA process itself suffers from basic errors like mislabeling or ineffective measures, the system becomes completely dysfunctional. This reflects not only operational negligence but also the erosion of quality systems and corporate culture. The failure of quality departments to prevent the closure of ineffective CAPAs, and even approving the release of known high-risk batches, demonstrates their loss of independence and authority. They have regressed from being "supervisors" to mere "rubber-stamp approvers."
3.2 Particulate Matter Deviation: Symptomatic Treatment Without Addressing the Root Cause and Recurrent Errors
Since February 2025, the company has experienced at least eight deviations related to particulate matter in finished products, with the products already in circulation. CAPA-25-003 was designed to address seven of these incidents, but its descriptions contradict the results of batch record audits. For instance, in the product batch 20250115, the first 100% inspection identified four minor defects, while the second inspection revealed one critical defect plus one minor defect. This indicates inconsistent and unreliable inspection processes. However, the quality department continues to release subsequent batches with similar particulate matter issues.
Deep-seated issues: Recurrent deviations indicate that root causes remain unidentified or unresolved. CAPA measures often remain superficial, addressing only isolated incidents without tackling systemic problems such as supplier management, component cleanliness, production process control, or internal inspection standards. The quality department's continued product release despite known issues and ineffective CAPA represents extreme disregard for patient safety, revealing how companies may compromise quality standards under pressure from production and release demands.
3.3 Quality Control: Inspections Lacking Scientific Basis
Observation 5 details the weak links in quality control:
Arbitrary visual inspection: After the initial inspection fails, multiple 100% re-inspections are conducted without scientific justification; the upper limit of AQL re-inspection frequency is arbitrarily set.
The process lacks standardization: multiple parties conduct the split without a documented procedure, and no impact on consistency has been assessed.
Deficiencies in infrastructure: absence of a defect database and lack of unified criteria for inspectors; prolonged failure to measure and record light intensity, resulting in uncontrolled inspection conditions.
The root cause lies in the erosion of scientific rigor in quality control. Visual inspection, as the critical release criterion for sterile products, relies on standardized protocols, stable conditions, and rigorous statistical analysis. Without these foundations, inspection results become meaningless, reducing release decisions to a gamble of subjective judgment. The absence of a defect database further exposes the company's failure to systematically accumulate and disseminate knowledge. Each inspector may operate with their own "personal standards," making consistent quality control impossible.
IV. The Total Collapse of Data Integrity and Quality Culture
4.1 Batch record review: Key information is intentionally or unintentionally overlooked
Observation 6 presents a typical case: A fentanyl/ropivacaine batch was released 43 days after production, and the supplier investigation report only confirmed that the particulate matter in the bags was polyamide and cellulose (wood fiber), with particles in contact with the solution. However, two AQL failure records related to this batch (identifying 8 units containing particles) and the deviation report requiring temporary batch retention prior to release were not thoroughly reviewed. This was not due to negligence but rather a systematic decoupling of release approval from quality control reviews.
Deep-seated issues: This highlights the critical flaws in the quality decision-making process. Batch release is not merely a document summary, but a comprehensive judgment based on all available quality information. Deliberately or habitually failing to review critical deviations and complaints prior to release essentially establishes a fragile barrier of "ignorance is bliss," which represents the collapse of the quality responsibility system.
4.2 Computerized System: Uncontrolled "Sharing" and Missing Tracking
Observation 8 depicts an IT environment with no data integrity whatsoever:
All employees have unrestricted access to and can modify core quality control documents, including environmental monitoring data and complaint records.
The software for batch release lacks electronic audit procedures and audit trail functionality.
The quality record form can be printed in unlimited quantities and cannot be verified.
The root cause lies in a fundamental breach of the FDA's ALCOA+ (Attributable, Clear, Synchronous, Original, Accurate, Complete, Consistent, Permanence, Available) principles for data integrity. Uncontrolled access permits covert modifications or deletions of data, while the absence of audit trails casts doubt on the authenticity of electronic records. Management admitted staff deliberately re-entered data to circumvent proper documentation protocols. This systemic failure transcends mere configuration issues—it reflects a toxic corporate culture that tolerates and even encourages data falsification.
4.3 Equipment and Materials: Overlooked Compatibility Risks
Observation 7 indicates that plastic turnover boxes used for transferring materials and products between clean areas are in direct contact with cleaning agents, but the company did not assess the risk of degradation and release of particles from the material after long-term exposure to cleaning agents.
Deep-seated issues: This reflects a lack of scientific rigor in supplier selection and material control. Any item that comes into contact with pharmaceuticals or may affect the production environment should undergo scientific evaluation regarding its compatibility, cleanliness, and durability. Neglecting such evaluation is equivalent to introducing an unknown and persistent risk source into the production process, which contradicts the "controllability" pursued in aseptic production.
Summary and Enlightenment:From Compliance to Quality Culture
The FDA 483 report of Park Avenue Compounding serves as a textbook case of systemic failure in quality management. It exposes a cascade of escalating issues:
1. Loss of technical control: Basic technical activities such as aseptic process validation, environmental monitoring, and cleaning and disinfection were not effectively implemented.
2. System-level failure: Quality management systems such as deviation management, CAPA, quality control, and batch release are either inoperative or operating in reverse.
3. Cultural layer decay: Data integrity is disregarded, scientific spirit yields to convenience, and quality is compromised by production pressure, ultimately leading to the breach of patient safety boundaries.
For the pharmaceutical industry, the warning of this case goes far beyond one company:
quality stems from design, but more importantly, from every operational step. Even the most flawless document system becomes a castle in the air if it fails to translate into employees' routine standardized practices and evidence-based decision-making.
risk management is a dynamic scientific process, not a static compliance document. It must be continuously updated based on real-time data and process knowledge.
The quality department must be independent, authoritative, and scientifically grounded. Its core mission is to safeguard patients, not to ensure compliance. When QA becomes a mere appendage of production, disaster is already brewing.
data integrity is the cornerstone of quality systems. Allowing data to go out of control is tantamount to acknowledging that all quality conclusions based on data may be false.
Ultimately, establishing a robust aseptic production quality system is a path without shortcuts. It requires an absolute commitment to quality from the highest levels of corporate management; it necessitates the integration of science, risk management, and patient safety into every process, decision, and employee's mindset. As evidenced by Form 483, Park Avenue Compounding and other enterprises with similar mindsets still have a long way to go to achieve this goal. For regulatory agencies and the entire industry, identifying and rectifying this systemic cultural corruption will pose an even more formidable challenge in safeguarding public health and safety.
Source: FDA official website: https://www.fda.gov/media/190024/download.
Disclaimer: This article is intended solely for knowledge exchange, sharing, and popular science purposes, and does not constitute commercial promotion, nor should it be regarded as medical guidance or medication advice. For copyright infringement, please contact us for removal.
Our product recommendations:
1.1367776-07-5 https://www.bicbiotech.com/product_detail.php?id=6472
2.1216026-07-1 https://www.bicbiotech.com/product_detail.php?id=6473
3.1092351-46-6 https://www.bicbiotech.com/product_detail.php?id=6474
4.1092351-41-1 https://www.bicbiotech.com/product_detail.php?id=6475
5.1367926-94-0 https://www.bicbiotech.com/product_detail.php?id=6476




