Genome sequencing is currently increasingly used in the diagnosis of lower respiratory tract infectious diseases, especially for the detection of pathogens. However, with the wide application of metagenomic sequencing (mNGS) technology, the clinical discovery of mNGS in the sequencing of fungi and mycobacteria requires high "wall breaking technology", and the technical difficulty is also greater. In addition, how to interpret the mNGS report, how to "guess" the effective sequence, how to verify the "guess" in the next step, how to extract the target nucleic acid sequence from a large number of pathogens to ensure the accuracy of the test results, seems to have become a difficult problem. Therefore, targeted sequencing (tNGS) technology has emerged. Due to its high sensitivity, high accuracy, low cost and relatively fast detection cost, targeted sequencing (tNGS) has high value in tuberculosis and tuberculosis drug resistance detection, identification of CSF pathogens, diagnosis of preterm lower respiratory tract infection and other fields. Then, how should metagenomic sequencing (mNGS) and targeted sequencing (tNGS) choose in the diagnosis process of lower respiratory tract infectious diseases? What are the advantages and limitations of these two technologies? Professor Lu Binghuai of National Respiratory Medicine Center of China-Japan Hospital gave a detailed interpretation in this lecture.
1. Selection and limitations of the mNGS technique
We are the following respiratory tract infections, which have a lot of pathogens, including viruses, bacteria, atypical pathogens, fungi, mycobacteria, etc. Different population, different seasons, different age stage, the etiology of the disease is not the same. With the conventional microbial culture detection methods, only a part of the pathogen can be cultivated. Because of the "weakness" of routine microbiological testing, many clinicians choose to bypass metagenomic sequencing (mNGS).
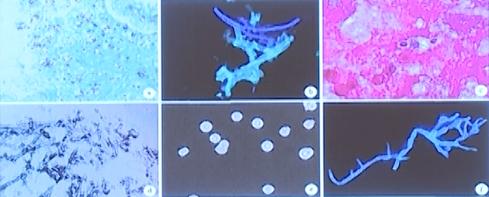
At present, mNGS is a very special technology that can detect all pathogens. Relatively speaking, the sequencing of viruses by mNGS is relatively simple and technically less difficult. However, for the sequencing work of fungi and mycobacteria, the requirements of "wall-breaking technology" are higher, and the technical difficulty is also greater.
At present, the increasing number of immunosuppressed population and the number of patients with invasive mycosis (IFD) are also increasing, causing a serious economic burden on patients. And as the lower respiratory tract infection of invasive candida, asergillus, pilus, Cryptococcus neoformans, pneumosporia carinii, local epidemic fungi, rare fungi such as detection rate is higher and higher, let clinicians headache problem is a lot of patients after the mNGS but found three or more fungi, mycobacteria amplification fragments, difficult to clear diagnosis. How to interpret the mNGS report, how to "guess" the effective sequence, how to verify the "guess" in the next step, how to combine the imaging results and clinical symptoms to improve the pathogen coverage, seems to have become the main theme of clinical MDT or consultation. How to extract the target nucleic acid sequence from a large number of pathogens and how to guarantee the accuracy of the detection results have become a difficult problem.
At the time of clinical diagnosis of infection, if the pathogen load is high, there is no problem with both traditional microbial technology, metagenomic sequencing (mNGS), targeted sequencing (tNGS). The problem now is how to analyze and interpret the mNGS test report when the pathogen load is low.
Another major problem with mNGS is to improve sensitivity and reduce specificity. The results of different companies are worse, unless there is more pathogen load. When the number of pathogens is low, different companies get very different results. In order to detect more pathogens, some specific databases also include non-specific fragments, which leads to the results after comparison with the database, not necessarily specific, still less clear diagnosis. Therefore, it is suggested that a secondary library should be built on the basis of the ordinary library to calibrate whether the amplified sequence is specific and whether the results are reliable. Take the sequencing of Mycobacterium, a group of slender, slightly curved, sometimes branched bacteria with a lot of lipids. Now many patients infected with COVID-19, influenza are prone to mixed bacterial infection or secondary Mycobacterium avium, Mycobacterium abscessus infection, need differential diagnosis. However, the mNGS results of such patients often show M. avium and M. abscessus, so it is difficult to determine whether the patients have secondary infection with mycobacteria.
2. "Traditional Microscopy Sliars and Culture" VS Metagenome Sequencing (mNGS)
(一)Microscopic smear microscopy: through intuitive observation, it can be seen that the inflammatory reaction of the human body, such as leukocyte aggregation and phagocytosis, can help to clinically identify the existence of pathogens, but the sensitivity is not high.
(二)Culture is the gold standard for infection diagnosis, but with a long time cycle. Cultivation of live pathogen is the premise of live susceptibility test:
1. Cryptococcus and Aspergillus are easy to culture;
2.Liquid culture is recommended for mycobacteria, which can improve the positive rate and shorten the reporting time.
Of all infectious diseases, more than 30% of respiratory infections, more than 40%~50% of bloodstream infections, and more than 50%~60% of encephalitis and meningitis cannot identify pathogens by traditional pathogen testing (direct examination, antigen testing, PCR, isolation and culture).
Common pathogens from which microbial cultures can isolate、

(3) The target of metagenomic sequencing (mNGS) is nucleic acid, which can report drug resistance genes
1. Carbapenemase resistance genes (for Enterobacterales);
2. mecA gene (for Staphylococcus);
3. Drug resistance genes of M. tuberculosis, etc.
Reading the results of mNGS from the perspective of traditional microbial testing shows that mNGS has been "expanded", and we need a method to calibrate the results of mNGS to determine whether it is reliable. If the basic microbiological detection ability of hospitals is relatively weak, it is difficult to solve this problem. In the context of mNGS application, how to develop the traditional microbial detection should, how to build and how to enhance is the focus rather than weaken. Many European and American countries mNGS is not fully rolled out, but their diagnosis and treatment work is carried out very well. From this point of view, the basic microbial detection ability is very important.
The mNGS has deepened the understanding of pathogens such as Chlamydia psittaci, human herpes virus (type 1 to 8), leptospira, rare NTM and Cryptococcus. However, whether the results of the database comparison are reliable, whether it is a pathogen, whether it is a pathogen that needs treatment, and whether it meets the criteria of infection, still need to be further explored. It is often more necessary to combine with traditional methods (conventional microbial microscopy with culture, histopathological staining, imaging, etc.).
3. Targeted sequencing (tNGS)
Targeted sequencing (tNGS), based on super-multiplex PCR technology, can carry out targeted pathogen detection, breaking through the limitations of pathogen detection.
(1) Specificity increase the number and proportion of nucleic acid sequences of target pathogens, increase the number of supporting reads and coverage of target microorganisms, and ensure the detection of difficult / demanding / low load pathogens.
(2) Detection of virulence genes: to improve the basis for distinguishing pathogenic bacteria and colonizing bacteria.
(3) Detection of drug resistance genes: compatible with the pathogenic pathogen and drug resistance phenotype.
Due to its high sensitivity, high accuracy, low cost and relatively fast detection cost, targeted sequencing (tNGS) has high value in tuberculosis and tuberculosis drug resistance detection, identification of CSF pathogens, diagnosis of preterm lower respiratory tract infection and other fields. Targeted sequencing (tNGS) represents an important development direction, especially in patients who do not need to detect too many pathogens.
4. Selection of metagenomic sequencing (mNGS) and targeted sequencing (tNGS)
(1) mNGS is of great help to the diagnosis of fever, unexplained infection or fever, excluding infection, and the diagnosis of rare, difficult, repeated and chronic infection
(2) TNGS can be used for grassroots groups / patients with common infections, including but not limited to various systemic community-acquired infections, hospital-acquired infections, etc. Ultra-multiplex PCR (forward enrichment) + high-throughput sequencing (NGS) targeted sequencing (tNGS) technology can meet 98% of the clinical application scenarios, and can realize the co-inspection of DNA and RNA without separate testing. It has the characteristics of fast (experimental TAT fastest 12h), sensitive (better sensitivity than mNGS), cheap (high cost performance), fixed (accurate quantification of pathogens).
(3) Lower respiratory tract infection requires a comprehensive diagnosis
Lower respiratory tract infection should be diagnosed comprehensively, combined with laboratory etiology detection, imaging, clinical symptoms, pathology, biomarkers and acute phase inflammatory response indicators. In the future of mNGS / tNGS / multiple molecular detection, we believe that:
1. <10 targets, small panel, can use fluorescent PCR technology (Gene Xpert);
2.10-50 targets, small and medium panel, using microfluidic POCT (Filmarry);
3.200-1000 targets, medium panel, available with panel tNGS;
4. No intended target, large panel, using mNGS.
brief summary
No technology can solve all the problems alone, mNGS / tNGS technology does not get rid of the limitations of nucleic acid detection, and the timely detection results need to be combined with traditional microbiological diagnostic technology and clinical comprehensive analysis and interpretation.




