Radiobiology is the science that studies the effects of radiation on living organisms. Its core goal is to understand the effects of radiation on cells, tissues, and whole organisms, and to assess their risks. With the expansion of nuclear energy applications and the popularization of medical imaging technology, the problem of radiation exposure has received more and more attention. Traditional methods of radiobiology research rely mainly on animal experiments and in vitro cell models. However, these methods have many limitations, such as ethical issues, and differences between experimental results and human physiology.
Organ chips (OOC) have been widely used in biomedical fields, such as regenerative medicine and precision medicine (Figure 1). The main advantage of OOC is the ability to build specific human models with organ or tissue functions, thus avoiding the use of animal models and greatly improving the new drug development process. An emerging application area of OOC is human internal irradiation research. Human internal irradiation studies lack a clear internal irradiation risk assessment model, and OOC technology can simulate the function of human organs or tissues, with great potential in radiobiology research.
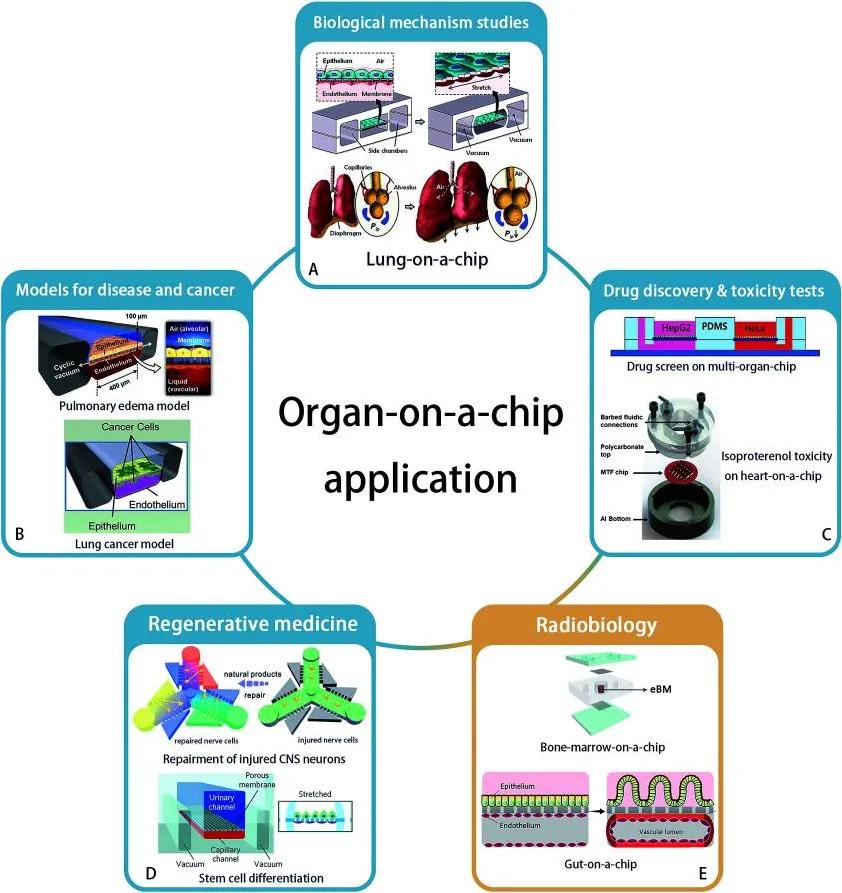
Figure 1. Application areas of OOC.
The application of OOC technology in radiobiology is still an emerging field. In 2011, Snyder et al first applied a microfluidic chip with liver tissue to this research field, confirmed the damage to liver tissue by space-like radiation and evaluated the therapeutic effect of the original drug amifoin. Recently, "intestinal chips" was applied to radiobiology studies by Jalili-Firoozinezhad et al. Their findings showed that γ -ray radiation exacerbated the generation of reactive oxygen species, cytotoxicity, apoptosis, and DNA breakage, disrupted the tight junctions and integrity of the intestinal barrier, and blurred the villus morphology. In addition, this intestinal model demonstrates that dimethyl alumoyl glycine (DMOG) may help prevent such damage from radiation (Figure 2).
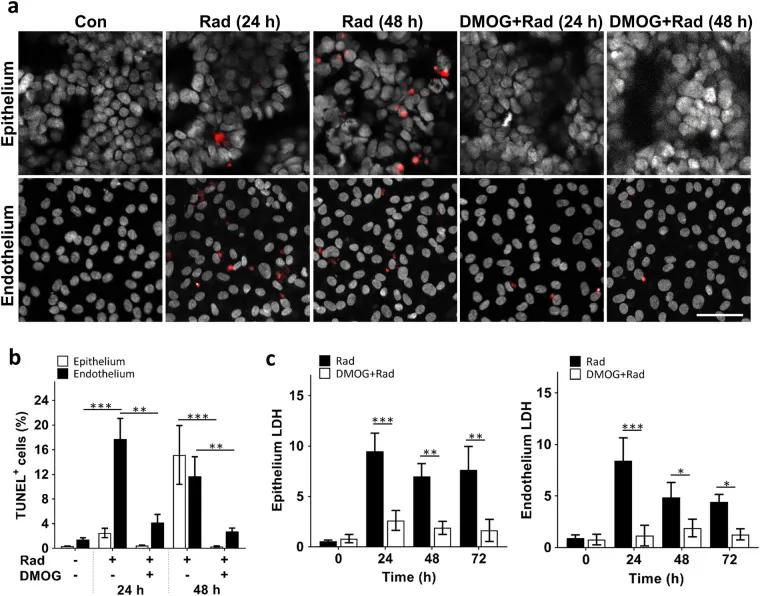
Figure 2. Radiation-induced apoptosis and cytotoxicity of intestinal epithelial cells and vascular endothelial cells, and the radioprotective effects of DMOG.
01 Application of organ chips in radiobiology
1. to simulate in vivo radiation exposure
Organ chips enable precise control of radiation dose and exposure time, thus simulating radiation exposure scenarios at different doses and times. For example, by designing a liver chip containing liver cells, the liver response at different radiation doses, including cell survival rate, DNA damage, gene expression changes, etc.
2. Study of multiple-organ interactions
Radiation affects not only a single organ, but also other organs through physiological and biochemical pathways in the body. The multi-organ chip (Multi-Organ Chip) can simulate the function of multiple organs simultaneously and study their interactions. For example, the combined microarray of the liver and kidney can study the effects of radiation on combined liver and kidney function and how radiation-induced metabolites affect other organs through the blood circulation.
3. High-throughput screening and personalized medicine
Organ chips have miniaturization and high throughput, suitable for large-scale radiation effect screening and drug evaluation. Furthermore, personalized radiotherapy risk assessment and drug screening can be achieved by using patient-specific cells. For example, by harvesting cells from a patient and growing them on a chip, the sensitivity of different individuals to radiation can be evaluated for personalized treatment options.
4. Simulation and control of the microenvironment
Organ-on-a-chip technology mimics complex in vivo microenvironments, including mechanical forces (such as blood flow shear forces), chemical gradients (such as gradients of oxygen and nutrients), and cell-cell interactions. This ability allows researchers to accurately simulate realistic physiological conditions under radiation exposure in an in vitro environment. For example, the lung chip can simulate the stretching and compression forces of alveolar cells during respiration, thus studying the effects of radiation on the respiratory system.
5. Dynamic monitoring and real-time analysis
Another important advantage of organ-chip technology is the ability to perform dynamic monitoring and real-time analysis. By integrating microsensors, researchers can monitor various physiological parameters within the chip in real time, such as pH value, oxygen concentration, and metabolite concentration. This real-time monitoring capability allows researchers to capture the cellular response after radiation exposure for dynamic biological analysis.
02 Advantages of the organ chip
1. Highly biomimetic: Organ chip can simulate the real human microenvironment, including three-dimensional structure, fluid mechanics and cell-cell interactions.
2. Reduce animal experimentation: The use of organ chips can reduce reliance on animal experiments, thus reducing ethical controversy.
3. Efficient and fast: The miniaturization and high-throughput characteristics of the organ chip enable it to conduct large-scale experiments and rapid data collection.
4. Personalized assessment: By using patient-specific cells, organ chips can achieve personalized radiobiological risk assessment.
5. High cost-effective: Because the experimental system of organ chip is usually small, the reagent and sample size are less, so the experimental cost is reduced. In addition, the high degree of automation, can save human resources.
Today, although radiation exposure in people's lives is limited to specific occasions, such as biomedical diagnostics, treatments, and even leaks from nuclear power plants, understanding the radiation-induced biological effects is still a key issue. Most of the exposure to low-dose radiation is in the body and can cause serious health problems. An increase in childhood leukaemia has been reported in coastal villages in Cumbria near the Sellafield nuclear facility. Unlike the clinical testing of drug candidates, radiation experiments cannot be performed directly in humans. Non-human organisms are often used directly as a model to study radionuclide metabolism. In the risk assessment of uranium inhalation, the incidence of cancer per radiation dose in animal models is comparable to that in the human body, however, it varies at different sites.
In order to overcome species differences in animal models and humans, OOC becomes a new platform for detection of radiologic effects. OOC can directly culture human cells for radiobiology studies, avoiding the use of animal models and differences in gene expression profiles such as transporters between species, all of which may lead to changes in response to low doses of radiation. With the help of OOC, early embryo and stem cell-derived embryonic tissues can be cultured and radiation diseases studied. The effect of radiation on individual health risk is influenced by age, sex and genetic background, so it is important to study the radiation biological effects of individuals, such as optimizing the dose of radiotherapy or radiation diagnosis to reduce the risk of subsequent malignancies. OOC can culture primary cells from individuals or specific populations to study individual injury responses. This is not only valuable for understanding the mechanisms of how low-dose radiation can induce biological effects, but can also be used to improve personalized medicine.
03 Future outlook
With the development and improvement of technology, the application of organ chip in radiobiology is promising. In the future, the organ chip is expected to be a standard tool for radiobiology research and risk assessment. Here are some possible directions:
1. Further development of multi-organ chips: In the future, multi-organ chips will be more complex and can simulate the interactions of more organs. By integrating more types of organ chips, researchers can more comprehensively study the effects of radiation on the whole organism.
2. Combine artificial intelligence and big data analysis: Artificial intelligence and big data analysis technology can help researchers to extract valuable information from a large number of experimental data, and improve the accuracy and efficiency of research. In the future, the combination of organ chips and artificial intelligence will promote the intelligent development of radiobiology research.
3. Further application of personalized medicine: By combining patient genomics, epigenetic and metabolomics data, the organ chip will provide a more accurate evaluation tool for personalized medicine and promote the development of personalized radiotherapy.
4. Development of new radiation protectors and therapeutic drugs: Organ chips can be used to screen and evaluate new radiation protectors and therapeutic drugs, so as to accelerate the development process of new drugs and provide more effective treatment options for radiation-exposed patients.
In conclusion, although OOC technology has not been widely used in clinical research, it has shown great potential in disease mechanism research, drug screening and even regeneration research. Similar to the success achieved in pharmacological studies, organ chips will be very useful in the field of radiobiology, especially the development of protective therapy after irradiation and the optimization of personal radiotherapy.
reference documentation:
1. Quan Y, Sun M, Tan Z, et al.Organ-on-a-chip: the next generation platform for risk assessment of radiobiology.RSC Adv.2020;10(65):39521-39530.
2. Jalili-Firoozinezhad S, Prantil-Baun R, Jiang A, et al.Modeling radiation injury-induced cell death and countermeasure drug responses in a human Gut-on-a-Chip.Cell Death Dis.2018;9(2):223.




